 There are so many benefits for saving the baby's cord and encapsulating the placenta by making placenta pills. Check out the information on Evidence Based Birth https://evidencebasedbirth.com/evidence-on-placenta-encapsulation/. Also download Dr. Shawn Tassone's presentation, The Two Way Umbilical Crd on LinkedIn. Slides describing the maternal-fetal bonding process prior to #birth that shows mothers when the fetus develops senses in utero. https://www.slideshare.net/ShawnTassoneMD/two-way-umbilical-cord
0 Comments
 The American College of Obstetricians and Gynecologists (ACOG) recently published Committee Opinion Number 736, released May 2018, which recommends Optimizing Postpartum Care. We birth workers and pre/post-natal yoga teachers have been talking about this “fourth trimester” and the importance of postpartum care for new mothers well after the birth of her baby and well beyond the typical 6-week postpartum check-up. “This Committee Opinion has been revised to reinforce the importance of the “fourth trimester” and to process a new paradigm for postpartum care.” In ACOG’s No. 736 Abstract (replaces No. 666, June 2016), the following published statements are especially exciting to me: “To optimize the health of women and infants, postpartum care should become an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs.” ACOG also discusses financial responsibility which may make Insurance companies’ eyebrows furrow, “Changes in the scope of postpartum care should be facilitated by reimbursement policies that support postpartum care as an ongoing process, rather than an isolated visit.” Here is where I start doing cart-wheels, “…the American College of Obstetricians and Gynecologists recommends that the timing of the comprehensive postpartum visit be individualized and woman centered. To better meet the needs of women in the postpartum period, care would ideally include an initial assessment, either in person or by phone, within the first 3 weeks postpartum to address acute postpartum issues. This initial assessment should be followed up with ongoing care as needed, concluding with a comprehensive well-woman visit no later than 12 weeks after birth. Insurance coverage policies should be aligned to support this tailored approach to the “fourth trimester” care (see Policy and Postpartum Care).” Whoah. I still do the ‘Happy Dance’ after I read that! Out of curiosity, has ACOG hired more women? I am happy to see ACOG finally coming on-board with a formal Committee opinion in an effort to change postpartum medical practice as well as affect policy changes for financial reimbursement. I haven’t been this excited over an ACOG opinion since they revised their decision about VBAC births! Although change make take time before we see it materialize into practice, this recognition of the Fourth Trimester is a step in the right direction! (Replaces Committee Opinion Number 666, June 2016) Bringing a child into this world can be one of the most rewarding experiences you will ever have as a woman. The idea of birthing a new soul and bringing life to our community is something most women have dreamt of since they were little girls.
However, having a child can also be very overwhelming with all of the tasks and things on your to-do list that must be done. Unless you have had a couple of children already and are a seasoned pro at this, you are going to have a lot of work on your plate that can feel a bit stressful (especially if you still have to work a full time job). This is where having a life coach can come in handy. While many people may assume or associate life coaching as someone who helps you “fix your life”, this is not fully accurate. While the coaching industry has made its name with helping people get their lives back on track, the truth is that a life coach uses certain techniques and skills to help their clients accomplish their goals regardless of their circumstances. Even the most successful executives, athletes, and Hollywood elite use coaches to support them. Some of the main methods a coach uses are: 1. Active Listening & Empathy This is where the coach is able to connect with their client on a deeper level to truly understand what it is they want to accomplish so they can help them find clarity and get unstuck. 2. Setting Goals Once the coach has helped you get clear on what it is you want to accomplish, they will then be able to assist you in identifying and prioritizing your goals. 3. Chunking After you have made a list of what your goals are, a life coach will help you break them down into bitesize steps so that they do not overwhelm you so that they are more manageable on a daily and weekly basis. 4. Support & Encouragement As you begin to tackle your goals on your road to success, there will be lots of twists and turns that come up that could potentially throw you off your game. It is now when your coach can provide support and encouragement so you can face your fears and overcome adversities. So to summarize, a life coach is someone who understands what you want to accomplish and supports you along that journey making the process easier and more enjoyable. Isn’t that what all moms need during their pregnancy? So if you are feeling a bit overwhelmed and scattered, try working with a life coach. Many professionals also offer online coaching services making it easy for you to gain access to them from the comfort of your home or smart phone. Contact Coach Sam at the Coaching Institute for more information: http://coachinginst.com/contact/  Midwife from Mexico, Naoli Vinaver Lopez, came to Los Angeles to demonstrate to the local doulas how to use the Rebozo for labor and delivery. In case you have not heard what a Rebozo is, essentially it is a Mexican shawl about about 4-5 feet in length, which serves many functions. Mexican women can wrap and carry their babies around their back or in a sling or pouch in front of the body. In labor, the Rebozo can help a woman with relaxation techniques and help progress labor and relieve pain. Angela from Rebozo Me Tenderly sells beautiful authentic Rebozos at a very reasonable price. Find Angela on Facebook RebozoMeTenderly. I keep a Rebozo in my doula bag and bring with me to every birth. The Rebozo keeps me warm in those very cold hospital rooms and can be used in a variety of ways during labor and delivery. Midwives and doulas can help correct a mal-positioned baby in order to help the baby rotate into proper anterior fetal position (tummy to mummy) and progress labor. What I learned at Naoli’s workshop, though, was about the “movement of sexual energy.” Of course! Birth is the manifestation of sexual energy. I just have never heard it described that way, as Energy. It makes sense then that when a woman is inhibited and her sexual energy blocked, labor would be longer and often more painful. Author Jennifer Vanderlaan of Birthing Naturally website has a great one-page description of the Rebozo and simple how-to techniques. Here is a short video clip on YouTube where Naoli and several doulas practice one Rebozo technique I like to call Sifting because it reminds me of sifting flour through cheesecloth. Watch this demo using a Rebozo (Mexican Shawl) in order to move Sexual Energy and progress labor. I reckon this particular movement might also help women with fertility blockages? If nothing else, it feels great! http://www.youtube.com/watch?v=Uyww8GZnT3k So pull out that Pashmina or Rebozo and move it, move it!  This is the year for VBACs in my doula practice. I love supporting VBAC mamas; they have this special zing and purpose about them. I suppose hindsight is 20/20 and so these women approach birthing, the second time, being more informed and prepared. In 2010, The American Congress of Obstetricians & Gynecologist (ACOG) issued Practice Bulletin No. 115, replacing Bulletin No. 45 which included the infamous requirement of doctors to be “immediately available” which resulted in a fire of VBAC bans to rage around the country, but primarily in rural areas. ACOG's current position is supportive of VBACs stating that VBAC is a “safe and appropriate choice for most women” with one prior cesarean and for “some women” with two prior cesareans. Being pregnant with twins, going over 40 weeks, having an unknown or low vertical scar, or suspecting a “big baby” should not prevent a woman from planning a VBAC (ACOG, 2010). That is great news across the country and I anticipate the Cesarean rate to low overall. The risk of uterine rupture with one prior low-transverse uterine scar is low, 0.5% to 0.9% so for those considering a VBAC, read Katie's inspiring birth story and the steps she took to ensure VBAC success! Katie’s VBAC Story – Birth of Rowan The Previous Cesarean From my 20-week ultrasound on, I knew that I would be having a scheduled Cesarean Section with our first baby girl, Daphne. Due to a defect in her abdominal wall that would require surgery, the doctors recommended that a Cesarean was the safest way for her to be born. I was heartbroken, fearing that it would pave the way for my subsequent births. Daphne’s birth was an emotional experience because there were so many unknowns about her health. I felt very detached from the birthing process, since I didn’t “birth” my baby. I was not an active participant in her birth at all. We got a brief glimpse of her after she was born and she was immediately whisked off to the NICU for evaluation and prep for surgery. It wasn’t until the next day that I got to hold her while she was hooked to monitors, IV’s, and tubes, and several days later began to breastfeed. While my C-section recovery was uneventful and fairly smooth, it was still a grueling and painful process. I couldn’t function normally for a long time and it took a significant amount of time for my body to heal. Selecting the Birth Team for the Second Pregnancy When we found out we were expecting our second baby, I knew immediately that I wanted something different from my first experience. I’ve always known and trusted my body to be an amazing thing, created with everything needed to successfully birth a baby. Even though it was explained to me over and over again by medical professionals that a C-section was just as safe as a vaginal birth, I felt that it couldn’t be, since my body was designed to birth babies. I felt like I had missed out on a fundamental part of being a woman by not being allowed to go through the process of birthing my baby and that I missed an important step in bonding with my baby in the process. Nearing the end of my pregnancy I searched the Internet for resources in the LA area and I kept coming across the names of several people who were active advocates for VBAC births, one of whom was a doula in the South Bay area named Patricia Grube. I had never heard of a doula before and began looking into it. As I talked things over with my husband, we decided that a doula would be instrumental in helping us achieve a successful VBAC birth by helping us navigate the complicated medical system and firm up our expectations and desires for birth. We chose Patricia as our doula after interviewing several doulas and felt she was the right fit for us. I became dedicated to attending her prenatal yoga classes at Yoga Works, which helped me prepare mentally, physically, and emotionally for the VBAC. I also knew that finding the right doctor and hospital would instrumental for a successful VBAC. Patricia and members form my church all recommended Dr. Donna Richey. She was respectful of my wishes to move around during labor and as a result, I believe the hospital staff, knowing her style and preferences, respected those more “alternative” aspects of my birth plan. Day One of Labor - Thursday On the morning labor began, I was awakened around 3:00 a.m. on March 7th with cramping and discomfort. I tried to shrug it off and ignore it, thinking and hoping it was just some indigestion or maybe some stronger Braxton Hicks contractions. They kept me awake on and off until morning when I realized they were coming every 10-15 minutes or so. I called Patricia then the doctor’s office. They requested I go to the hospital for an initial reading to verify I was in labor. I went to the hospital with mildly uncomfortable contractions, which they ended up timing at 7-10 minutes apart, but with only fingertip dilation and 60% effaced. Meanwhile, my husband, Van, made arrangements to return home from his business trip and to be home by that evening. I continued with the same cramping feeling throughout the day, with some a little more intense than others and the pressure and discomfort increasing through the evening. Since it was still quite manageable, I decided to drive to the airport to pick up Van, however, during the hour that I ended up driving around and waiting for him in the car, the discomfort intensified. We made it home and decided to head to bed and get whatever rest we could. After going to bed at about 11:30 p.m., I woke up around midnight, unable to manage the contractions lying down. I decided to let Van sleep and managed early labor on my own, finding that being on my feet was the most comfortable. I tried to sleep on the couch, sitting up a little and also leaning over the arm of a large comfy chair to preserve my energy. I spent the time blowing up my birth ball and testing it out to manage contractions. I took a warm bath and had candles lit around me to help me relax, which was wonderfully soothing. I eventually determined that the most comfortable thing for me was to lean against something while doing a figure 8 with my hips. Day Two of Labor - Friday As Friday morning approached, I began timing the contractions again and felt they were getting more consistent and uncomfortable. By late morning, Patricia made her way over to our house. My 2 ½ yr old daughter had woken up and was bouncing around the house, climbing on me during contractions and wanting to play with the birthing ball. With everyone awake and lots going on, my contractions spaced back out to about 7-10 minutes apart. Van cooked me some breakfast and continued to do hip squeezes through each contraction. His support was amazing throughout the labor process. He rubbed my shoulders, stroked my face and caressed my back and arms. He was constantly by me and I didn’t want him anywhere else. We slow danced through a lot of contractions with me hanging on his shoulders. Patricia suggested we try to nap. Van and I both reclined on the couch a bit and were able to nap briefly—about 30 minutes, before contractions began waking me again. Daphne and my cousin left, and I was able to relax a little more, knowing that Daphne was taken care of and would not be a distraction. I remember trying hard to focus on the contractions being productive and bringing me closer to my baby, rather than the discomfort I was feeling. Patricia had recommended listening to my relaxing playlist that I had put together with jazz and classical. I enjoyed singing along to some of my favorite songs. I remember crying with joy as Van and I embraced and I looked at our family photos on the wall, realizing that soon there would be another sweet little girl to add to them and that what I was experiencing was bringing her closer to us. I also cried joyfully as I listened to the words of Iz’s version of “What a Wonderful World” when he sings about babies crying and watching them grow, excitedly anticipating our new little one. Patricia suggesting that we try going up and down the stairs. My body fell into a pretty good routine of getting through one trip up and down before I would have a contraction. I was breathing heavily through each one and vocalizing to help me manage it. Patricia was wonderful, giving me suggestions of things to do to help labor progress a little more quickly and help with my comfort. When I would start to lose control during contractions, she would help me to focus and clam myself by reminding me to breathe, keep my vocalizing grounded and low instead of high pitched, and often moaning along with me. It was hard to know what I wanted and what would help me, but each of her suggestions were wonderful, from food, to music, to essential oils to ease nausea and give energy. I remember feeling discouraged as the evening wore on and the hours went by and things weren’t progressing very quickly. I was getting exhausted but was petrified to lie down since it seemed that it brought them on more strongly. I also started to feel a great deal of pelvic and rectal pressure. I told Patricia and she had me sit on the toilet for several contractions, when finally I started to have some bloody show. The contractions were 3 to 4 minutes apart and we decided to make our way to the hospital. We arrived at about 10:00 p.m. and I was dilated to 4 ½ centimeters, 75% effaced, and -1 station. My night nurse was wonderful, allowing me to move around freely while still being hooked up to the monitors. She also never once asked me to rate my pain or about pain medication. My contractions were continuing to get stronger and more painful, sometimes lasting several minutes and I was starting to feel extremely tired. Day Three of Labor – Saturday, Birth Day! In the early morning hours, as I was laboring on the birth ball with Van behind me to support me, I was falling asleep between intense contractions. I would nod off and Van would catch me and make sure I didn’t fall. I began to feel as though there would be no way I would make it to the end if it weren’t close. I told Van and Patricia that I really wanted to consider the epidural and asked the nurse to check me to see where I was. I was at 6cm with a bulging bag of waters, having progressed only 1 cm from the last exam I had had 4 hours previous. Since things were progressing so slowly, we decided to go ahead with a light dose epidural, which allowed us all to rest for several hours. The night shift doctor came in to see me before her shift ended. She discussed breaking my water in order to progress labor. She said several things that seemed threatening about my lack of progress and needing to hurry things up or they’d need to do a C-section. She asked how big my baby was estimated at…luckily Dr. Richey had not recorded an estimate on my chart. This doctor tried to find my water bag, and was unable to locate it. I had felt several gushes throughout the evening and perhaps my waters already broke? We discussed the possibility of doing a small dose of Pitocin, but I decided to wait a little longer. My contractions had spaced again to 4-5 minutes apart. My new nurse Fereshteh (which means “angel”) came in to do a vaginal exam and I was dilated 7-8 cm and the baby was at zero station! I remember loving my epidural because I could still feel and move my legs, but was relieved of the pain. I could still feel intense pressure, however, which I preferred so that I could know how things were progressing. By 10:45 a.m. I was beginning to feel intense rectal pressure like I needed to go to the bathroom. A vaginal exam showed that I was 8 ½ cm dilated and 100% effaced. At this time Patricia had me on my side moving my leg up and down, hoping to open things up. I focused on relaxing and visualizing my cervix opening and the baby moving down. My contractions continued to be spaced a little further out than was desirable as I was continuing to feel increasing pressure, and Patricia and I discussed the benefits of introducing a low dose of Pitocin to bring them closer together to help with the pushing phase. At 11:45 a.m. they gave me the lowest dose of Pitocin and my contractions quickly moved to every 3 minutes apart. By noon, I felt stronger rectal pressure that I had read about in other birth stories and knew that I needed and wanted to push. I was asked to blow through my contractions, which in my mind at the time was the most ridiculous thing anyone could request of me, the urge to push with them was so very strong. I was checked and I was 9 ½ cm dilated. Ferry turned off the Pitocin and by 12:15 p.m., I could no longer hold off pushing. Ferry checked me again and I was finally dilated to 10 cm and the baby was at +1 station. The new hospitalist, Dr. Mimi Hong was not available as she was delivering another baby and I was again asked to blow through several more contractions. I was angry and remember shooting a death glance towards Patricia, who whispered to me that anyone could catch the baby. Blowing through the contractions was impossible and I ended up pushing through parts of several I was asked to resist. Finally, at 12:25 p.m. Dr. Hong became available and I was told I could actively push. I did so on my side for a while and then in a semi-reclined position. During this time my epidural was turned off, although I hadn’t felt like it was doing too much in the time prior to that. The Final Push! As we waited for the pushing contractions to start, I remember looking up at Van and saying that maybe God would bless us to have a short pushing phase since the rest of my labor had been so very long, and silently praying that it would be so. Although I could fully feel the contractions coming on, all I wanted was for the nurses and Patricia to tell me when to push and for how long. It was wonderful to hear them cheering me on and telling me what a great job I was doing. I couldn’t care less who was in the room or what else was going on, I was very focused on just pushing and getting my baby girl here as quickly as I could. It was still very surreal to me that it was really happening. They gave me oxygen as one point during the pushing process, which helped me to breathe more deeply. After one of my pushes they all said they could see the head. I could feel it, like a bowling ball between my legs, but again, it was difficult to grasp and I remember asking if she was really there. Patricia told me to reach down and touch her head, which I did. It helped give me motivation and strength for those final pushes. Right before my final contraction that brought her out, my playlist got to one of my favorite songs from labor, Iz’s version of “What a Wonderful World/ Somewhere Over the Rainbow”. On March 9th, at 12:49 p.m., our baby girl Rowan Jane Willis was born! She weighed 8 lbs, 13 oz and was 21 inches long with a 14” head! They placed her directly on my chest where I could cuddle her and look at her. I was still in disbelief, but it was heavenly and we were elated. The doctor allowed the cord to pulsate completely before Van cut it and I was able to easily deliver the placenta without any Pitocin. The baby breastfed right away on her own and it was lovely to just be together and delaying all routine baby interventions until after the Golden Hour. We are thrilled to have her here and especially grateful that our VBAC Birth Plan was so closely followed and respected and that things went so well considering the circumstances. My recovery has been amazing in comparison to my c-section and I really felt back to normal, minus the sleep deprivation, after about 2 weeks! I know that we were guided in this process to the right people to help us achieve a peaceful, healthy birth for our baby. I’ve been reflecting on the whole process and am amazed by the positive feelings I have about it all, despite the pain I experienced and how long and exhausting it was. I have been thinking back fondly on how grateful I felt for everyone that helped and supported me during labor. I felt such intense love for Van as he supported me through such a long process and watched me go through such a physically intense experience. I am so grateful for the experience I had and especially for the sweet baby girl that it brought to our family! [Originally posted April 7, 2013]  There are many questions to encourage dialogue between you and your doctor, especially when you are still interviewing a medical care provider. Here are my TOP 5 suggested questions that will give you a good idea as to the doctor’s philosophy about caring for you and supporting your Birth Preferences. Ask these questions in a respectful and non-confrontational manner to illicit a healthy dialogue with the doctor. It is a good idea to interview at least 2 or 3 providers. Listen to your Intuition and watch the doctor’s body language. And if during the course of your pregnancy you are getting the feeling your doctor may not be on the same page as you regarding your Birth Preferences, it may not be too late to change providers. It may not be too late to ‘break up with your doctor!’ Please check with your insurance company regarding switching doctors because some insurance companies may have time-deadline restrictions.
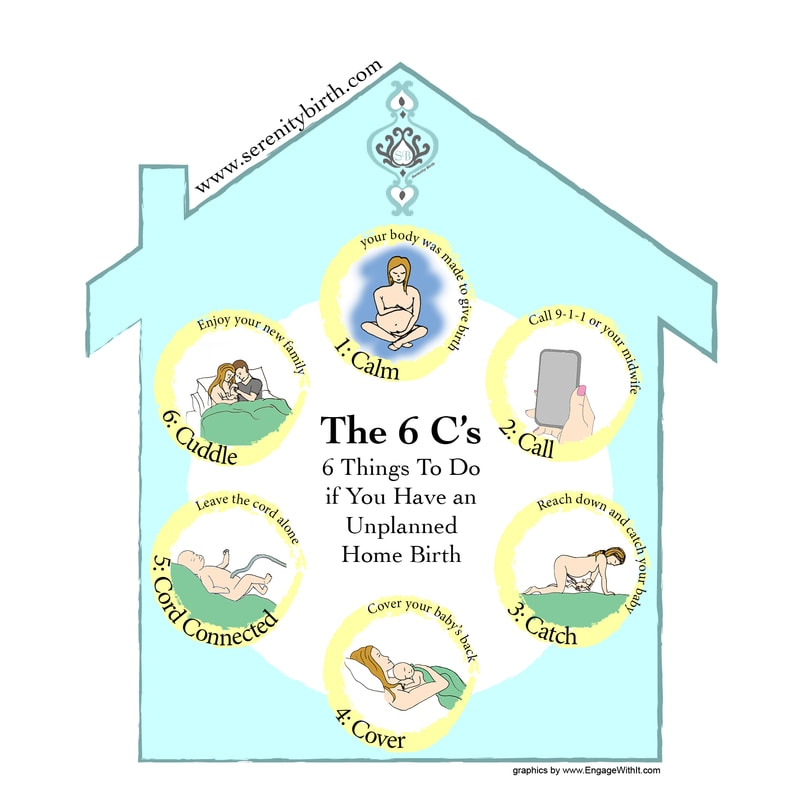
Wishing you happy memories on your Labor Day. May you experience a Serenity Birth! Follow me on Instagram: Serenity_Birth, Twitter @Serenitybirth1 [Originally published May 17, 2015]  We’ve all heard stories about the baby born in the car, on the way to the hospital or born unassisted (unintentionally) at home. We call it precipitous labor (a labor length of under three hours). While the intention of these couples was to give birth in a hospital facility or planned home birth, the fact of the matter is that birth happens! I once heard Ina May Gaskin say at a birth conference, “Birth was made to work in case nobody is there.” Although precipitous labors occur more frequently with subsequent births, the overall percentage of this happening to you is very LOW so no need to rush to the hospital at the sign of your first contraction. Here are a few statistics I found from the CDC 2004 report. The overall percentage of labors, which were deemed Precipitous: In discussing this topic with my midwife friends, Ashley Guntkowsi, CNM and licensed midwife Amy Tinney and Certified Nurse Midwife, MaryLou O'Brien, here are the top six things to do in the rare case that a fast birth should happen to you. I call it the 6 C’s: 1) Calm yourself, breathe and stay put. Don’t freak out, no need to ‘boil the water’. Stay calm and take a few deep breaths. Remind yourself your body was made to give birth. 2) Call 9-1-1 for emergency paramedics or call your midwife if you had planned on a home birth. I personally do not recommend getting into the car to drive to the hospital under these circumstances. It is wiser to stay put and let the professionals come to you rather than risk giving birth in transit. 3) Catch the baby. Lower yourself closer to the ground or get on the bed. Reach your hands down towards your vagina to catch your baby. Then pull your baby onto your chest. Your partner or family member can do this too; just tell them it is like catching a slippery football. Note: if you have a doula present she may not catch the baby. I repeat, your doula may NOT catch your baby. Many women experience the same sensation as their baby is crowning that they do when needing to have a bowel movement, which may prompt you to sit on the toilet. If this happens, reach down to touch your vagina – if you feel the baby’s head, stand up! 4) Cover the baby. Keep the baby warm! Babies are born quite wet, but have an easier time breathing when they are dry and warm. Immediately place the baby on your chest or tummy to help regulate your baby’s body temperature. Use a dry towel, jacket, or even plastic bag to cover your baby’s exposed backside. Of course what you use is dependent on what you have handy. 5) Cord connected AND left alone. Leave baby’s umbilical cord alone until medical staff reaches you. As for clamping and cutting, there’s no hurry. The placenta is still attached inside of mom for a few minutes. The cord extends out of the vagina and into baby’s belly button while the baby breathes on her own. Unless your placenta falls out on its own, your midwife/doctor will help you birth it once you are all in the same place. In fact, some mamas opt for a Lotus Birth, leaving the placenta and cord in tact and connected to the baby for days until the cord dries up and disconnects on its own. 6) Cuddle with your baby. Enjoy the time of being skin-to-skin with your baby and connecting as a new family. Soon the paramedics (or midwife) will arrive to assess the well-being of you and your baby. In most cases the paramedics will still transfer you to the closest hospital however some doctors will “allow” you to stay home based on satisfactory report from the paramedics. Now, take a deep breath in and EXHALE.. Let’s recap the 6 C’s to assist you in case of a precipitous birth:
That’s really it! Stay calm. Trust birth, and carry-on. I will leave you with this inspiring birth story of a yoga student’s precipitous birth at home!
|
|






 RSS Feed
RSS Feed